The real challenge with weight loss is keeping it off.
When you lose a significant amount of weight, the body does what it can to return to its original weight and the further from the original weight you drop, the greater the pressure to rebound. The body seems to have a functional weight set point that it defends irrespective of the extent of its internal stores of energy (in the form of fat). The set point can be raised by factors that affect the body’s homeostatic mechanism of weight maintenance. While this set point can be raised, it does not seem to be amenable to being lowered.
Take the example of someone who has gained weight due to pregnancy. The new higher weight is encoded as a new set point and if they then try to lose weight below this set point, the body counters with adaptive physiological processes that evolved to defend itself from starvation. These include the following mechanisms.
- Thyroid function changes. Reverse T3 increases, T3 and T4 decrease, effectively rendering you hypothyroid
- Muscle efficiency increases (improved muscle function per calorie, less wasted calories)
- Neuro-humoral changes: leptin, CCK, peptide YY all DECREASE, thus removing inhibitory actions on ghrelin, increasing appetite
- Decrease in resting energy expenditure due to weight loss and less available metabolically active tissue
- Adaptive thermogenesis decreases resulting in reduced resting metabolic rate
- Decreased sympathetic tone (and increased parasympathetic tone) result in less fat mobilization, slower physiology.
The result of these processes is that it is increasingly hard to maintain the new lower weight. As a consequence, fewer than one out of six people who have lost a significant amount of weight can keep it off after a year. The forces that return weight to the set point can be opposed by bariatric surgery and by anti-obesity medication.
There is a concern that by weight cycling, you end up resetting your basal metabolic rate lower across all weights. So even after you regain the weight, you are still burning fewer calories, even at rest. Why might this happen?
With weight regain, the body’s imperative can be understood as follows: it seems to want to reconstitute fat free mass (FFM). This includes lean muscle but also the weight of organs, bones and other non-fatty tissues in the body. In Keys’ famous Minnesota weight loss experiment with conscientious objectors to WW2, over-eating and weight gain did not abate until FFM was replenished. During weight regain, there was a desynchronization in the reconstitution of fat mass and fat free mass, so subjects ended up with an overshoot of fat return. What this means is that when you regain the weight, you end up with an increased percentage of fat as compared to muscle. Fat is a less metabolically active tissue and so you should theoretically have a lower BMR at the new weight, and this is what is observed. So to be clear, not only do you regain weight, you end up with a slower metabolism for having lost it in the first place.
So consider the typical dieter who, while losing weight, will lose both fat and FFM (muscle, for our purposes). As they regain the weight, they will regain primarily fat. So functionally, they are replacing muscle with fat. Not all their muscle, but enough that it affects their BMR.
Where does the set point reside?
How is this set point encoded and where does it reside in the body? This turns out to be an enormously complex issue that is informed by the multiple variables that influence appetite including hormone signaling, homeostatic networks in the midbrain, bioenergetics related to mitochondrial metabolism, genetics, developmental epigenetic factors, the food reward circuits in the striatum, physical activity, and larger factors such as stress and socioeconomic forces. This is a long way of saying we don’t know. But let’s consider three theories.
- Leptin resistance: the adipocyte-secreted hormone leptin increases in proportion to the amount of body-fat. Reduction in body fat reduces the amount of circulating leptin, which triggers feeding behavior. Conversely, an increase in leptin does not trigger reductions in intake unless the organism is leptin deficient. Therefore leptin may represent a mechanism to protect against fat loss only. Supplementing with leptin has not been shown to be a valid weight loss strategy.
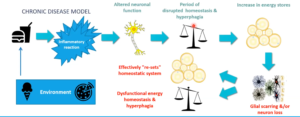
- Maybe there is a ponderstat–an actual sensor in the hypothalamus. Possibly more specifically, in the arcuate nucleus of the hypothalamus, where the major nuclei relevant to maintenance of weight reside. One theory is that specific astrocytes in the arcuate nucleus either sense changes in nutrition or somehow are attuned to loss of weight, possibly in relation to leptin levels. Alternatively, over nutrition induces an inflammatory reaction that changes neuronal function and resets the homeostatic system (as in the figure above). Increased energy stores are encoded in a process known as reactive gliosis.[i]
- Mitochondrial theory: we know that mitochondria are irrevocably degraded by obesity. Oxidative damage associated with obesity damages them, reducing their effectiveness and their numbers. As a consequence, metabolism slows. The consequence of widespread mitochondrial dysfunction, metabolism has been functionally reset because we are not using as much fuel, we cannot use it because we don’t have the mitochondrial capacity. So with diminished energy use, there is a trend toward defending a higher weight.
- Changes in the microbiome: we know that dietary restriction changes the microbiome and that those changes affect the degree to which the gut absorbs fat or lets it pass through the enteric tract. Changes in the microbiome composition predispose (at least mice) to increased regain of fat after dieting. There does not appear to be clear evidence yet in humans.
But then how do we keep the weight off?
- Bariatric surgery uniquely evades some of the post-weight loss changes related to a set point, but only for a time and then not completely. The commonly performed surgeries change the composition and concentration of bile-acids, which are important signals of satiety. Also, because of structural changes in the gut, more nutrition passes to the distal part of the intestine causing increases in anorexigenic hormones such as GLP1 and PYY (hindgut hypothesis). There may also be changes in direct signaling to the CNS. Then the mechanical issues: the stomach is smaller, there is a fear of dumping syndrome if you eat too fast, etc. All of these factors contribute to a functional reduction in the set point, at least temporarily. Yet many people who achieve weight loss after bariatric surgery subsequently regain some or much of the weight.
- Pacing. One basic principle is that if you must lose large amounts of weight, then do it slowly so that the body gradually adjusts to a lower set point. Losing weight more deliberately and pausing between plateaus seems to help people evade the set point phenomenon and thus maintain reduced body weight,[ii] though to be clear, this finding is anecdotal, controversial and lacks experimental proof.
- Muscle. When you lose weight, you lose both fat and fat free mass. Fat free mass includes the weight of organs and other tissues, but also muscle. When you regain the weight in the context of increased muscle mass, you will regain fewer pounds of fat. In other words, muscle mass will protect against fat regain. There are medications that should be used to mitigate the set point or even reset it. Ultimately, weight loss needs to be done in a controlled fashion with a plan, with frequent pauses to permit the body to catch up. Muscle mass facilitates this process.
- Dietary characteristics. I suggest a weight loss diet that is somewhat less palatable, with less sugar, salt, fat and calorie density, more fiber. The diet will be satiating but less rewarding. If you can stick to a diet like this for a few weeks, it will change the brain reward centers and alter how you defend adiposity.
- Mitochondria: theoretically increasing the health and number of mitochondria will increase resting energy expenditure and may reset an elevated set point for the rationale suggested above. This would be done by zone 2 exercise and a variety of supplements that support mitochondrial biogenesis. Also mitophagy inducers such as fasting and rapamycin. In the future, maybe mitochondrial transplantation will be possible.
- Rapamycin: speaking of the namesake mtor inhibitor, it has been shown in rats to durably reset the ponderstat by unknown mechanism.
- Microbiome: there is animal evidence that referring with a high protein concentration mitigates post weight loss fat regain.[iii]
- Finally, no discussion of weight is complete without a mention of exercise, sleep and stress management, the famous lifestyle triumvirate. Changing these often seems so inaccessible to people who are locked in patterns of work, parenting and life-responsibilities.
[i] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6977167/pdf/main.pdf
[ii] https://www.nature.com/articles/ijo2017224
[iii] Zhong, W., Wang, H., Yang, Y. et al. High-protein diet prevents fat mass increase after dieting by counteracting Lactobacillus-enhanced lipid absorption. Nat Metab (2022).
Also https://www.sciencedirect.com/science/article/abs/pii/S001650851730152X
